By the end of 2021, 95 percent of American workers considered changing jobs. Of these, 92 percent were so ready for advancement they were willing to change industries to find a position better aligned with their goals. Dubbed the “Great Resignation,” this trend thrust employers into a fierce competition to keep talent from migrating to other companies.
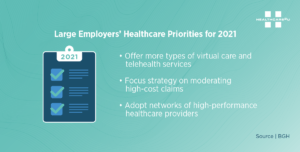
While flexible work schedules and remote work found themselves at the top of the most valued benefits list, peace of mind regarding healthcare is still top of mind for most. The pandemic health crisis reemphasized the importance of having access to affordable healthcare for families of all sizes.
Non-Salary Benefits are Key
Employees are taking a closer look at non-salary benefits as talent acquisition and retention grow increasingly competitive. Employers must consider the cost of providing quality benefits, meeting the needs of employees, and creating a great culture. Premium health benefits help reduce absenteeism and boost morale, but companies are finding it more and more difficult to balance costs with quality.
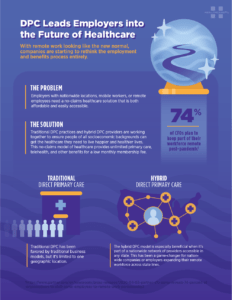
Benefits brokers have the ability to think holistically about how different benefits options work together in a health plan. This expertise provides a unique opportunity to educate employers and HR professionals on products that can reduce overall costs. One of these products is direct primary care (DPC).
Direct primary care works in harmony with traditional benefit options like HDHPs, MECs, and more. By reducing claims exposure for employers, DPC can effectively reduce the costs of a health plan while allowing an employer to provide more comprehensive benefits. The benefits of a direct primary care membership far outweigh the costs. They include more customized healthcare, better overall health, unlimited access, and substantial cost savings.
Customized Healthcare
Because direct primary care is not health insurance, DPC providers are not limited to the time constraints that accompany major insurance providers. Doctors can spend more time learning about a patient’s family history and previous medical conditions. This more personalized approach can help providers detect conditions before they escalate to an unmanageable or extremely costly stage.
Unlimited Access to Care
Most DPC memberships offer in-office as well as virtual care. Technology has made it possible for members to access a healthcare provider 24/7/365 for little to no out-of-pocket costs. This benefit is extremely valuable to millennials and Gen Zers.
Substantial Cost Savings
With a DPC membership, employees can avoid high deductibles and copays to get the care they need. Costs with a DPC provider are transparent, so there are no surprise fees after a visit. Employers also enjoy significant savings because there are no insurance claims generated whenever an employer seeks care from a direct primary care provider.
Make Yourself More Valuable
Every broker wants to grow his book of business and help his current clients achieve their benefits goals. The best way to make an impact is to provide real solutions that help employers reduce costs while making their current talent and recruits feel seen and cared for. By educating employers on the benefits of adding direct primary care to a health plan, brokers can make themselves more valuable to present and future clientele.
Contact Healthcare2U for more information and helpful resources to educate clients on direct primary care.